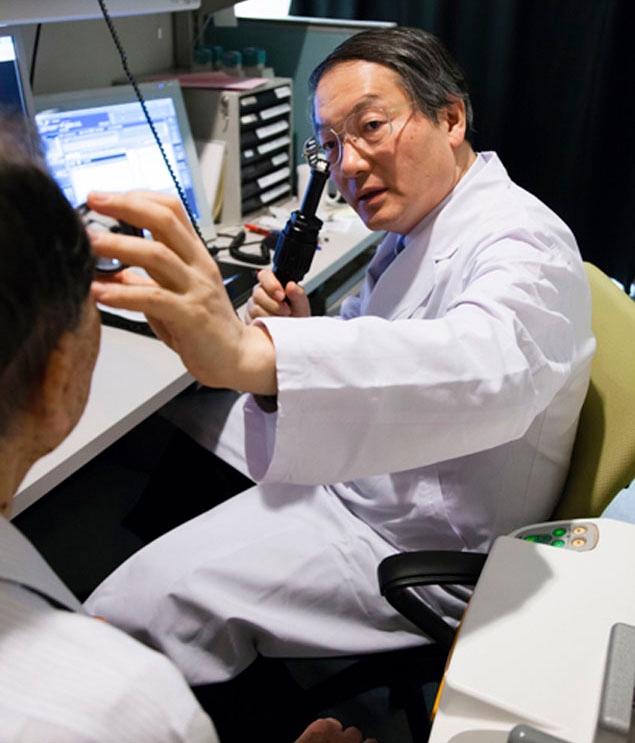
Ophthalmologist, Dr.Takayuki Akahoshi
(Mitsui Memorial Hospital)
Ophthalmologist Continues to be the World’s Preeminent Provider of Cataract Surgery
While his primary objective was to lecture at a Tokyo university and attend international conferences, he also had a more important, private agenda: to undergo cataract surgery at Mitsui Memorial Hospital, in Tokyo’s Chiyoda Ward.
For that operation, Mahathir relied on the world’s leading authority on cataracts, Dr. Takayuki Akahoshi.
No One to Take on Surgery For an Ultra-VIP
In fact, there weren’t.
At age 90, Mahathir suffered from diabetes, heart disease and a number of other conditions, making even straightforward cataract surgery highly risky. At home and abroad, every doctor he consulted turned him down, and the only one who agreed to perform the operation was Dr. Akahoshi.
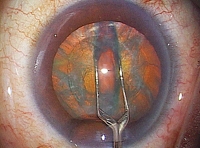
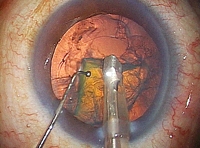
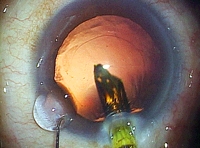
What made this difficult surgery possible was a procedure developed by Dr. Akahoshi in 1992 called the Phaco Prechop method. As the name indicates, this technique involves pre-chopping the phaco, or internal lens of the eye, prior to ultrasonic emulsification and aspiration. The surgery can be performed on an outpatient basis with a minimal physical toll: it requires an incision of just 1.8 mm, can be completed in three or four minutes, and results in zero bleeding. Not only is it safe and effective, but no other cataract surgery results in less strain on the body. This method enables Dr. Akahoshi to complete surgery in less than a minute and a half for each eye, a boon for patients who have difficulty remaining in a prone position for extended periods of time.
Ordinarily, the procedure used in Japan involves applying ultrasound to the lens of the eye in its whole state, requiring a lengthy 10 to 30 minutes; this generates heat, which along with pressure on the eye during surgery creates a significant strain on the cornea and the optic nerves. The incision can be as large as 3-6 mm, and because it requires stitches, can easily lead to distortion of the eyeball and post-operative astigmatism. Dr. Akahori has succeeded in solving all of these problems with his procedure.

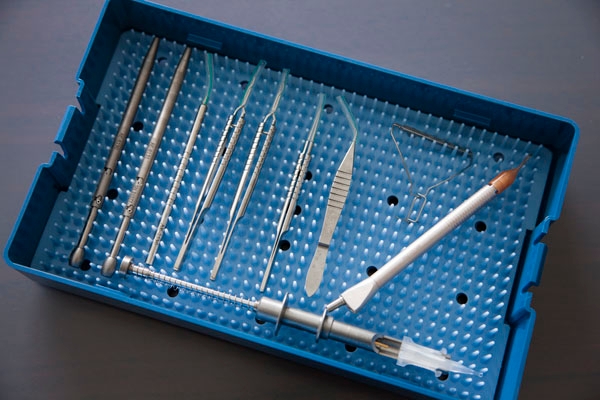
With the goal of ensuring the best possible operation, this operating room is designed down to the smallest detail specifically for cataract surgery. On busy days, Dr. Akahoshi will perform as many as 60 operations here.
“With so many people waiting for surgery, I must perform as many operations as I can. Still, we never know what might happen, so I leave myself room to take on 10 more if need be.”
Twin Operating Rooms, The Ultimate in Ingenuity
“For the patient, cataract surgery is a once-in-a-lifetime operation. We always do our best to eliminate anxiety, and to ensure that the patient is relaxed and able to undergo the finest procedure possible,” says Dr. Akahoshi.
Part of that effort is represented by Dr. Akahoshi’s twin operating rooms. These were designed to enable him to move back and forth between them, safely and efficiently performing an astounding 60 cataract operations a day, and upwards of 9,670 procedures a year (in 2014). The two units are connected, with a pre-op preparation room between them; each of the units has the same equipment and instruments arranged the same way, and identically composed surgical teams stand by in each room.
“Good afternoon, Mr. A. Are you nervous? Don’t worry, this won’t take long.”
After a few gentle words to the patient laid out on the operating table, Dr. Akahoshi begins surgery. Since only topical anesthesia is used, the patient remains awake and is able to talk.
First, using a specially designed ultra-thin diamond scalpel, the doctor opens a 1.8 mm incision in the cornea. There is no bleeding. Next, he uses a special tool called a prechopper to quadrisect the lens, which is a cloudy white due to the cataract, before using an ultrasound oscillating tool that looks like a microscopic vacuum cleaner to break up the lens prior to emulsification and aspiration.